
Mr Mark Ashworth FRCS (Orth)
Consultant Orthopaedic Surgeon
HIP AND KNEE PAIN
Femoro-Acetabular Impingement(FAI)
What is FAI?
There is an abnormality in the shape of the ball and socket of the hip joint. The ball (femoral head) of the hip joint grates/impinges against the socket (acetabulum). Symptoms may include restriction of movement, clicking of the hip joint or pain.
The impingement causes repeated minor damage to the cartilage lining the hip joint and to the seal around the edge of the acetabulum (labrum). This results in tears of the labrum (which can be painful) as well as cartilage damage and early hip arthritis.
FAI can be seen with joint hyper-laxity and is also associated with low back pain. It is possible for both hips to have FAI.
Why has it taken so long to get my diagnosis?
Because only minor damage occurs with each impingement, it takes many years for the damage to become bad enough to cause pain. So it can take a while to be recognised by the patient and often longer still before they find someone who understands how to treat this condition.
However, some patients with FAI complain only of stiffness and restriction of hip movement but not pain. Progressive loss of motion in the hip can be associated with ongoing FAI. (Speak to your specialist about this).
FAI as an identifiable condition is very new. Most GPs have not heard of it. Some physiotherapists and general orthopaedic surgeons are unaware of FAI. Specialist hip surgeons have a better understanding of this condition.
How many types of FAI are there?
There are 2 types of impingement, but most of the time, the Cam and Pincer forms exist together.
-
Cam impingement- the femoral head is not perfectly shaped. Either the head is not round or the head-neck junction lacks the usual recess for the edge of the acetabulum to safely sit in. This causes abnormal contact between the head-neck junction and the edge of the acetabulum.
-
Pincer impingement- results in the labrum being pinched/injured between the edge of the acetabulum & the front of the head-neck junction. Either the front edge of the acetabulum is too long or the acetabulum faces slightly backwards instead of its usual forward position. Occasionally pincer impingement is because the acetabulum is too deep.
Cam impingement video
Pincer impingement video
How is it diagnosed?
Most cases are diagnosed from a good history & examination with tests used to confirm where the problem is in the joint.
-
Hip pain – (groin, side, or back of hip) usually after exercise or in hip flexion e.g. squatting or during intercourse.
-
Loss of hip movement/stiffness.
-
Catching, clicking & giving way of the hip.
-
Examination for hip pain in hip flexion with the shin rotated to the outside (flexion to 90deg, adduction 20deg+ & full internal hip rotation) = impingement test.
Can back pain be a sign of FAI?
While not well understood, patients with FAI often have low back pain, localized to the sacroiliac joint of the pelvis. Treating the FAI can relieve the back pain.
The following may be confused with FAI
Low back pain
Trochanteric bursitis
Piriformis syndrome
Sports hernia (abdominal muscle strain)
Groin or thigh strains
Iliopsoas tendinosis
FAI pain typically does not go beyond the level of the knee.
What tests are usually performed?
X-ray shows the shape of the femoral head & acetabulum and can also show arthritis. But, x-ray does not always demonstrate the FAI abnormality. Our hip FAI x-ray policy is for:-
‘Standing AP Pelvis and Lateral hip (cross table in 15deg internal rotation)’.
Cam prominence on front of hip
AP Pelvis
Lateral hip


Calcified labrum, a sign of labral injury

Prominent posterior
wall a sign of pincer impingement

Usually an MRI scan of the hip is ordered. The scan involves an injection of gadolinium ‘dye’ into the hip joint (under local anaesthetic) to show the labral tears. The scan involves lying still inside the scanner tube for about 20 minutes. A measurement from the ‘radial MRI sequence’ determines how much Cam impingement exists on the femoral head-neck junction (the Alpha angle). The larger the Alpha angle, the larger the Cam impingement lesion. The scan also demonstrates the pincer abnormality when present.
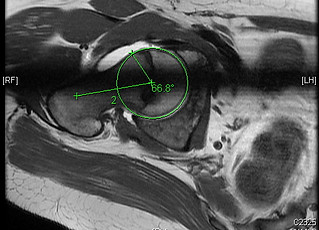
MRI showing abnormal alpha angle
Occasionally, an MRI will be reported as “normal”, yet the clinical history and examination indicate FAI. In this situation, further investigation with an examination under general anaesthetic & hip arthroscopy (key hole surgery) may be needed.
The MRI is also helpful in excluding other causes of pain including avascular necrosis (dead bone) and tumors.
Occasionally a CT (CAT) scan is needed this can show the bone edges clearly if the MRI does not.
What causes FAI?
It is not yet clear whether FAI begins at birth or develops during periods of growth. It is believed that it is due to a combination of genetic & lifestyle factors:-
-
It is possible that very athletic teenagers (before the skeleton stops growing) have an increased risk of FAI.
-
Contact sports such as football are associated with Cam impingement.
○FAI is not mild Developmental Dysplasia of the Hip (DDH)
DDH generally refers to too little coverage of the head by the acetabulum, where as FAI generally refers to too much coverage of the head by the acetabulum. Both DDH and FAI are associated with labral/cartilage tears.
What types of treatment exist for FAI?
-
Non-operative management – A less active lifestyle, possibly with cortisone injections, physiotherapy advice or rest. (Although a good physiotherapy program focusing on hip strengthening may be beneficial, the stretching associated with yoga may make the symptoms worse).
-
Surgery – FAI causes tears of the labrum. These can be treated by cutting out the torn tissue. Although this often relieves the pain it may not protect from the ongoing damage started by the FAI.
-
Some surgeons can remove the FAI abnormality during arthroscopy.
-
Open hip debridement is an alternative non keyhole operation. All aspects of FAI can be treated this way.
My labral tear was treated with a hip arthroscopy, can I still have FAI?
If you still have pain, you may have underlying FAI. This can cause ongoing damage to the hip joint.
How long should I wait before seeking treatment?
Any wait may result in further injury. Discuss this with your specialist.
Is it sensible just to wait a few years and have a total hip replacement?
Yes, if your current symptoms are tolerable. The postoperative rehabilitation from a total hip replacement is significantly less than an open FAI operation. However, rehabilitation after arthroscopic surgery is much less arduous than after open surgery or hip replacement.
But, the lifespan of a hip replacement is usually shorter the younger the patient- i.e. those who tend to have FAI.
Does FAI lead to permanent damage?
It is believed by most FAI experts, but not yet proven, that this is a pre arthritic condition; in effect this FAI ‘abnormality’ starts the process of arthritis. Others believe that what we see on the scans is the arthritis process already having started. Those in the first group believe that surgery on the ‘abnormality’, if done early enough, should reduce the risk of developing arthritis. Those in the second group do not claim this.
What happens during the surgery for FAI?
1. Hip arthroscopy (key hole surgery):-
This is performed as day case surgery in most cases. The hip joint is distracted up to 15mm using an orthopaedic traction operating table &, through 2 to 4 small incisions, an arthroscope is placed into this gap in the hip joint to assess & treat the damage.
If repair of a torn labrum is not possible, only the damaged part is removed. Not all hip arthroscopists are able to perform removal of the FAI abnormality and repair of a damaged labrum.
During hip arthroscopy, 2 compartments of the hip are visualized-
The central compartment – is composed of the surfaces of the femoral head and the acetabulum as well as the soft tissues (i.e., labrum & ligamentum teres).
The peripheral compartment – is the remainder of the hip joint and refers to the area along top & front of the femoral head and neck.
•How long does a hip arthroscopy take?
If this is for removal of damage, but no repair and no bony ‘FAI surgery’, it usually takes less than 1 hour.
If labrum or cartilage repair and FAI surgery occurs, it may take about 2 hours.
•What is the main benefit of hip arthroscopy FAI treatment?
Arthroscopic surgery, unlike open surgery, does not need the hip joint to be dislocated, so recovery time is quicker.
-
What are the main complications of hip arthroscopy FAI treatment?
These are uncommon but include:-
-
DVT/PE (blood clot)
-
Inability to get the telescope into a tight joint
-
Scuffing of the surface cartilage by the telescope
-
Infection
-
Not removing enough FAI bone
-
Nerve injury (e.g. Lateral Cutaneous nerve of the thigh, Sciatic or Pudendal).
-
Injury to perineum due to the pressure from the traction device
-
Femoral neck fracture (very rare)
-
AVN (dead bone) of the femoral head (very rare indeed)
2. Open surgical hip dislocation:-
This involves a cut on the side of the hip (approximately 20 - 30cm depending on buttock size), an osteotomy (bone cutting) of the trochanter of the upper thigh bone to gain access to the hip joint and protect the blood supply to the hip. Then, dislocation of the head from the acetabulum exposes all parts of the joint. This exposure allows treatment of labral tears and the FAI abnormality of the head and acetabulum. The piece of bone (trochanter) is then replaced and permanently held with 3 screws.
•How long does open FAI surgery take?
All aspects of this surgery can typically be done in 1 ½ hours.
•What are the main risks of open FAI treatment?
Complications from FAI hip surgery are uncommon but include the following:
-
DVT/PE (blood clot)
-
Femoral neck fracture
-
Infection
-
AVN of the femoral head (dead bone)
-
Non-union (failure of the healing of the osteotomy)
-
Nerve injury (e.g. Sciatic or Pudendal)
-
Further surgery to remove prominent/uncomfortable screws
-
Up to 1/3 have some degree of abnormal bone formation in soft tissues
-
Scarring/Adhesions
What is the recovery/rehabilitation from FAI surgery?
Your postoperative activity level depends on your surgeon’s recommendation, the type of surgery performed, and the condition of the hip joint at the time of surgery. Usually:-
-
Stand up on day of surgery using crutches.
-
Average 2 day stay after open surgery to allow for good pain control and to learn the rehabilitation exercises
-
6 weeks touch-weight bearing walking using crutches.
-
Active hip exercises as instructed by the physiotherapist.
-
For open FAI surgery, 0 - 2 weeks -only simple passive exercises allowed.
-
-
@ 6 weeks - X-ray and clinic review, if the bone is healing/healed satisfactorily you will then increase to full weight bearing immediately (for arthroscopic surgery), or over the next 2 weeks and then dispense with crutches (for open surgery).
-
@ 12 weeks a further check x-ray may be taken.
What are the results of FAI surgery?
The early results are very encouraging with excellent pain relief. Initially some find progress very slow with weakness and aching for up to 3 months. Then good progress is seen with most people recovering well by 6 months after surgery. However, it is expected that you will have the odd ache for up to one year after the operation.
Arthroscopic surgery results
-
In one study of 158 patients, symptoms disappeared in nearly all the patients. Most reported a 50% reduction in pain by 3 months improving to 95% reduction in pain after 1 year. Three patients required a total hip replacement after an average of 22 months.
Open hip surgery results of 4 studies
-
In a study of 213, most patients had an improved range of movement and less pain 2 or more years after the operation.
-
‘Good or excellent’ result seen in 26 out of 29 hips.
-
After 5 years, 15 out of 23 patients had working hips and had not needed another operation.
-
Patients treated with labral repair/re-fixation had a significantly better overall clinical outcome at 2 years.
What type of treatment is offered?
-
Physiotherapy
-
Cortisone injections
-
Open FAI surgery
-
Arthroscopic surgery- offered to all bar the most severe cases
Comments by the National Institute for Clinical Excellence (NICE) on FAI:-
NICE states that the benefits & risks of FAI surgery are uncertain. This does not mean surgery should not be done, but that your doctor should fully explain the surgery, risks and the benefits to you. There are no long term results, so NICE insists that the effectiveness of this surgery is monitored. For this reason you will need to fill out a scoring form before and at regular intervals for some years after your operation.
Our current policy is to assess you with an x-ray and scoring system pre operatively and then post operatively, at:-
6 weeks; 12 weeks; 1, 2 and 5 years.
All adverse events should be documented and details forwarded to the National Patient Safety Agency's (NPSA) National Reporting and Learning System.
NICE information guidelines on arthroscopic FAI surgery https://www.nice.org.uk/guidance/ipg408
NICE information guidelines on open FAI surgery https://www.nice.org.uk/guidance/ipg403